By Richard Cunningham, OSU M4 // Edited by Michael Barrie, OSU EM Attending
Case:A 54 year old woman with a history of diabetes mellitus type 2, obesity, kidney stones and multiple episodes of pyelonephritis presents with flank pain. It started 3 days ago, has been constant, and intermittently increases in severity. She rates the pain as 4/10. The pain is described as a dull ache, at times sharp, and radiates to the right upper quadrant. The patient endorses some nausea but denies fever, emesis, diarrhea, constipation, chest pain, SOB, dysuria and hematuria. Upon further questioning she says this feels very similar to the times she had kidney infections. She has no history of abdominal surgeries.
Her vital signs are within normal limits and she is afebrile. On exam, she is comfortable appearing and has mild CVA and RUQ tenderness. Her abdomen is soft without guarding or rebound. The rest of her exam is benign.
After reviewing the above case, what is the one lab test (not including imaging) you would order? If you think like me, you would go straight for the UA. Flank pain, history of kidney stones and pyelo, it’s got to be a slam dunk, right? Wrong. Her UA was significant for only trace protein. Well shucks, looks like she’s heading to the CT scanner.
What is your backup diagnosis now? The pain did radiate to her RUQ and she is obese; maybe she has gallbladder pathology? Wrong again…
This woman had appendicitis confirmed on the CTAP.
Atypical Appendicitis:
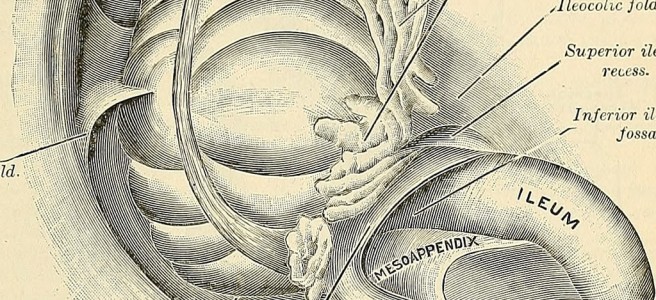
Appendicitis is a common surgical condition traditionally managed with early appendectomy and is associated with low morbidity and mortality. The classic presentation is vague peri-umbilical pain that migrates to the right lower quadrant; this however only accounts for about 50% of patients. The others vary in their presentation due to the age of the patient, the position of the appendix and coexisting conditions such as pregnancy. Retrocecal appendices can be shielded from the anterior abdominal wall by overlying bowel, leading to less severe pain in a non-classic location. A gravid uterus can push the appendix higher into the abdomen, leading to RUQ pain. These atypical presentations can lead to delays in diagnosis and treatment, so it is important to remain vigilant and keep a broad differential.
Some other learning points to consider include being wary of the chief complaint of flank pain. When I see this in the chart I automatically think of the kidney, mainly stones and infection. But it is critical to keep in mind what other pathology can lead to pain in this area and keep a broad differential: low back strain, rib fracture, AAA rupture, zoster of the thoracic dermatomes, pulmonary embolism, cholecystitis, and of course, appendicitis (among others).
Also keep in mind that when the patient tells you when gathering the history that this feels like a condition they have had before, do not let that pigeon hole you into that diagnosis. Stay broad, be creative in constructing your differential. It very well may be a recurrence of that same condition, but sometimes it won’t be and you will get burned. Remember one of the 10 Commandments of Emergency Medicine: Trust No One.
Take home points:
- 50% of patients with appendicitis presents atypically (it’s normal to not be normal!)
- Infants and elderly patients are more likely to have atypical presentations
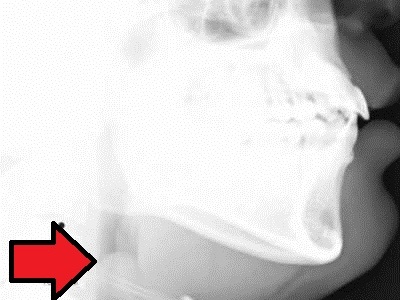
- Patients with a retrocecal appendix will have more flank pain
- Pregnant patients will have pain in atypical locations depending on trimester.
- In flank pain, always keep a broad differential!
References:
Liu CD, McFadden DW. Acute abdomen and appendix. In: Greenfield LJ, et al., eds. Surgery: scientific principles and practice. 2d ed. Philadelphia: Lippincott-Raven, 1997:1246–61.
Ong EMW, Venkatesh SK. Ascending retrocecal appendicitis presenting with right upper abdominal pain: Utility of computed tomography. World Journal of Gastroenterology : WJG. 2009;15(28):3576-3579. doi:10.3748/wjg.15.3576.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2715990/